- Back to Home »
- No more chemo? It may happen

- "Targeted therapies" may be changing the way we treat cancer
- Cancer cells can sometimes mutate to overcome the drugs' effects
- The new approach could mean gentler and more tolerable cancer treatments
- Chemotherapy may become the treatment of last resort
(CNN) -- There's a revolution occurring in cancer treatment, and it could mean the end of chemotherapy.
When it comes to taming tumors, the strategy has always been fairly straightforward. Remove the offending and abnormal growth by any means, in the most effective way possible.
And the standard treatments used today reflect this single-minded approach -- surgery physically cuts out malignant lesions; chemotherapy agents dissolve them from within; and radiation seeks and destroys abnormally dividing cells.
There is no denying that such methods work; deaths from cancer have dropped by around 20% in the U.S. over the past two decades. But as effective as they are, these interventions can be just as brutal on the patient as they are on a tumor.
 Marines inspired by cancer survivor
Marines inspired by cancer survivor  Cancer patient to cancer doctor
Cancer patient to cancer doctor 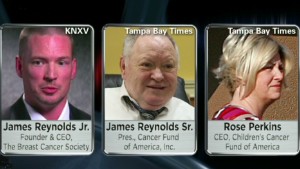 Beware of these cancer charity rip-offs
Beware of these cancer charity rip-offs So researchers were especially excited by a pair of studies published in the New England Journal of Medicine last week that showed a new type of anti-cancer drug, which works in an entirely different way from chemotherapy, helped leukemia patients tally up to an 83% survival rate after being treated for two years.
TIME.com: On the horizon at last, cancer drugs that harness the body's own immune system
The report was only the latest to emerge since 2001, when imatinib, or Gleevec, the first drug to veer away from the take-all-comers approach on which cancer therapies have been built, accomplished similar improvements in survival for patients with chronic myeloid leukemia (CML) and gastrointestinal stromal tumor (GIST).
Could the end of chemotherapy be near?
"It's a question we are all asking," says Dr. Martin Tallman, chief of the leukemia service at Memorial Sloan Kettering Cancer Center. "I think we are definitely moving farther and farther away from chemotherapy, and more toward molecularly targeted therapy."
It's the difference between carpet bombing and "smart bomb" strategies for leveling an enemy -- in this case, a fast-growing mass of cells that can strangle and starve surrounding normal tissues.
Targeted therapies, as they are called, are aimed at specific pathways that tumor cells use to thrive, blocking them in the same way that monkeying with a car's ignition, or it's fuel intake, can keep it from running properly. The advantage of such precise strategies is that they leave healthy cells alone, which for patients means fewer side effects and complications.
TIME.com: Self-sabotage: Why cancer vaccines don't work
"The field is moving toward using the right drugs at the right time in the right patients," says Dr. George Demetri, senior vice president of experimental therapeutics at the Dana Farber Cancer Institute. "We're moving toward a more precise understanding of cancer, and being able to tailor therapies toward an individual's cancer."
In the case of the NEJM studies, researchers were able to target an active receptor on immune cells responsible for enticing them to grow out of control, blocking the protein and essentially shutting down two different type of leukemia tumors.
Already, patients diagnosed with GIST can avoid chemotherapy altogether, thanks to Gleevec. "No patient diagnosed with GIST should be getting chemotherapy today," says Demetri.
Patients who develop certain types of lung cancer or melanoma caused by a cancer-promoting mutation known as BRAF are also starting to replace toxic chemotherapy agents with new, more precise medications designed to thwart the BRAF pathway.
And a study presented at the most recent meeting of the American Society of Clinical Oncology showed for the first time that a chemotherapy-free regimen led to a higher survival rate after two years than traditional chemotherapy for acute promyelocytic leukemia, a cancer of the bone marrow.
The refined approach does have a weakness, however. Cancer cells, like bacteria and viruses, are wily enough to bypass roadblocks to their survival, and often mutate to overcome the effects of targeted drugs. That's the case for a small percentage of patients on Gleevec.
But even that shortcoming isn't insurmountable. With growing knowledge about the molecular processes that drive tumor biology, researchers are able to design medications that thwart cancer cells' attempts to bypass medications. It's all about staying one or two steps ahead of the cancer, and already, researchers are testing drugs that address Gleevec resistance and hoping to widen the resistance gap.
"The field is moving so fast that there are new drugs already being developed to tackle new resistant clones," says Tallman. "(Resistance) is a concern, yes, but it doesn't negate our excitement about the future."
TIME.com: Inside America's drug shortage
Working in the doctors' -- and patients' -- favor is the fact that cancers aren't monolithic entities composed of the same abnormal cell copied thousands of times over. Individual tumors may be composed of different types of aberrant cells, possessing a variety of mutations that are susceptible to different drugs. And this cast of cells can be ever-changing over the course of an individual patient's battle with the disease.
While such heterogeneity and unpredictability could, on one hand, make tumors too daunting to tackle, they also represent an opportunity to employ an entirely new way of fighting tumors.
Traditionally, if a tumor developed resistance to a chemotherapy agent, doctors would have abandoned it completely and moved on to another drug or another treatment strategy. But now they are able to biopsy tumors and perform more sophisticated genetic and molecular tests that help them to decide, for example, that the bulk of a tumor remains susceptible to a targeted therapy while only a small portion has become resistant.
They can then either remove the resistant portion surgically or add another targeted therapy to tackle just that portion while keeping the patient on the original regimen that will still treat the remainder of his cancer.
"That's a new concept," says Demetri. "That didn't exist before targeted therapies."
TIME.com: The screening dilemma -- Health special: Cancer
For patients, these types of creative strategies could mean gentler, more tolerable cancer treatments, and more years of living cancer-free. Combinations of drugs may become the norm, much as they have become the standard for treating HIV infections.
So far, says Dr. Scott Kopetz, associate professor of gastrointestinal oncology at MD Anderson Cancer Center, refined targeted therapy cocktails appear to work best for blood cell and immune cell cancers like chronic leukemias that tend to be more homogenous from the start, making them susceptible to the newer drugs.
Solid tumors such as those in the breast, prostate and lung generally contain a wider variety of genetically different cells even at diagnosis, which makes them more challenging -- although not impossible -- to treat with targeted drugs.
"Where there is a lot of genetic heterogeneity, such as in most solid tumors, there is more headwind we have to fight against, more opportunities for rapid resistance to develop," says Kopetz.
That means that for the time being, chemotherapy may remain part of the cancer doctor's arsenal -- and even these agents are being revamped to cause fewer side effects. New ways of encasing the toxin in fat-based bubbles or linking it to nano-particles that deliver the drug just to the tumors while bouncing off of healthy cells are making regimens more tolerable.
Increasingly, though, chemotherapy may become the treatment of last resort, rather than the first wave as some basic truths about cancer are being knocked down and rewritten. For instance, it may not be as helpful to treat cancers by where they originate -- in the breast or prostate or lung -- but rather by the processes that fuel them.
That's why a targeted drug developed to treat melanomas is now used to suppress lung cancers, and why genetic and molecular analyses of tumors are becoming more critical to match the right medications to the right cancers.
"Many, many fundamental concepts in cancer are being challenged now based on new information," says Tallman. "Of course that is leading to major shifts, paradigm shifts in treatment approaches, and ultimately, I think, better care patients and better outcomes."
This article was initially published on TIME.com .
No more chemo? Doctors say it's not so far-fetched
© 2012 TIME, Inc. TIME is a registered trademark of Time Inc. Used with permission.







